Blood Can Be Very Bad! - How to Read an Emergent Head CT
/The cranial computed tomograph (CT) has assumed a critical role in the practice of emergency medicine for the evaluation of intracranial emergencies, both traumatic and atraumatic (trauma, stroke, subarachnoid hemorrhage, intracranial hemorrhage).
A number of published studies have revealed a deficiency in the ability of emergency physicians to interpret head CTs. Nonetheless, in many situations the emergency physician must interpret and act upon head CTs initially without assistance from other specialists.
Some things can wait for Nighthawk / radiologist reads . . . some things can’t.
A 2009 study showed only 50% of CT studies read by teleradiology were completed in 60 minutes.
The emergency physician should be able to rule-in or rule-out life threats identified on CT and act on them.
CT scan Basics
Hounsfield Units
Bone is the most dense = +1000 Hounsfield Units
Air is the least dense = -1000 Hounsfield Units
Water is in the middle = 0 Hounsfield Units
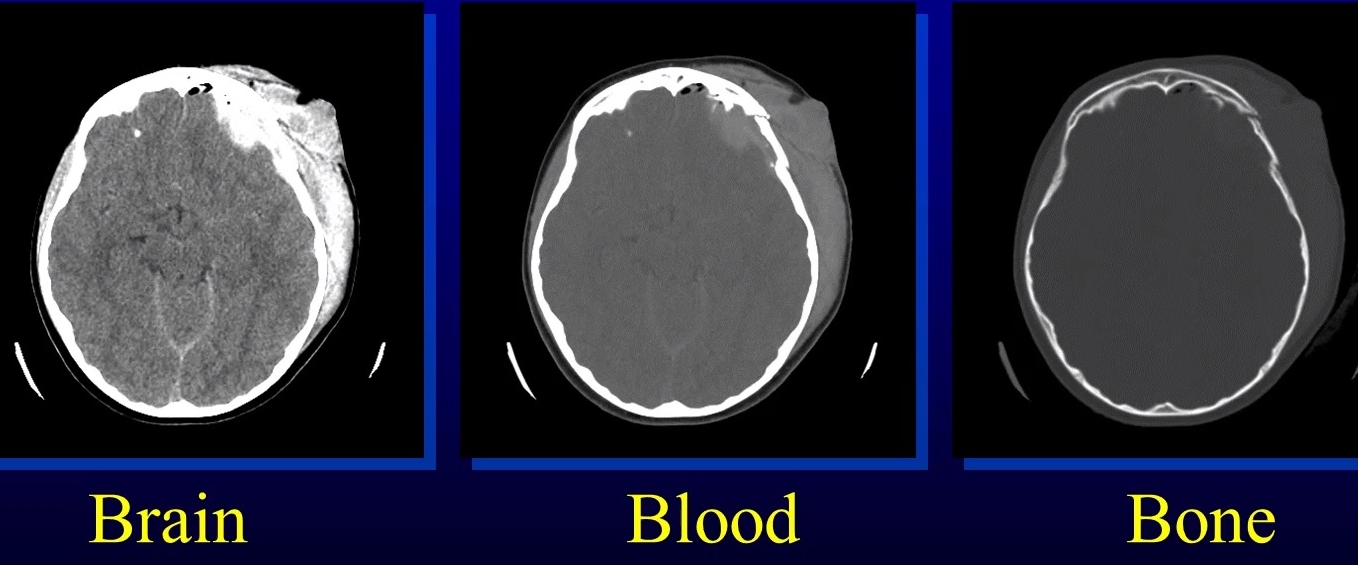
Windowing
Windowing allows the CT reader to focus on certain tissues on a CT scan that fall within set parameters.
Tissues of interest can be assigned the full range of blacks and whites, rather than a narrow portion of the gray-scale.
With this technique, subtle differences in tissue densities can be maximized.
different windowing for brain, blood and bone
Blood can be very bad
Utilizing a systematic approach is one way that the clinician can ensure significant neuropathology will not be missed.
Just as physicians are taught a uniform, consistent approach to reading an ECG (rate, rhythm, axis, etc.), the cranial CT can also be broken down into discreet entities, attention to which will help avoid the pitfall of a missed diagnosis.
One suggested method to avoid missing an emergent diagnosis is to use the mnemonic “Blood Can Be Very Bad”. In this mnemonic, the first letter of each word prompts the clinician to search a certain portion of the cranial CT for pathology: Blood = blood, Can = cisterns, Be = brain, Very = ventricles, Bad = bone.
B(lood) is for Blood
Ask yourself three questions:
Is blood present?
If so, where is it?
If present, what effect is it having?
Epidural Hematoma
Lens shaped
Does not cross sutures
Classically described with injury to middle meningeal artery (but source can be venous)
Low mortality if treated prior to unconsciousness (< 20%)
Subarachnoid Hemorrhage
Blood in the cisterns/cortical gyral surface
Aneurysms responsible for 75-80% of SAH
AVM’s responsible for 4-5%
Vasculitis accounts for small proportion (<1%)
No cause is found in 10-15%
20% will have associated acute hydrocephalus
Subdural Hematoma
Typically falx or sickle - shaped
Crosses sutures but does not cross midline
Acute subdural is a marker of SEVERE head injury (mortality approaches 80%)
Chronic subdural usually slow venous bleed and well tolerated
Intraventricular Hemorrhage (IVH)
Can be traumatic, secondary to IPH with ventricular rupture, or from subarachnoid hemorrhage with ventricular rupture (especially PICA aneurysms)
IVH is present in 10% of severe head trauma
Associated with poor outcome in trauma (may be marker as opposed to causative)
Hydrocephalus may result regardless of etiology
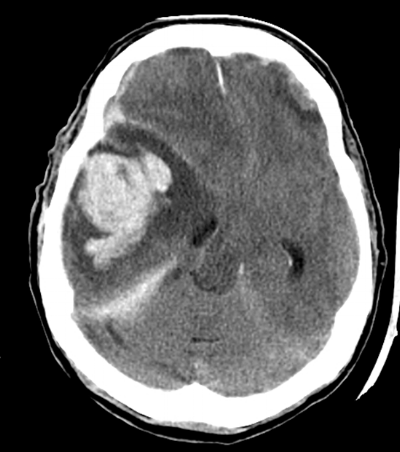
Intraparenchymal Hemorrage (IPH)
Seen as high-density areas on CT, usually with much less mass effect than their apparent size would dictate
Nontraumatic lesions due to hypertensive disease are typically seen in elderly patients and occur most frequently in the basal ganglia region
Hemorrhage from amyloid angiopathy is frequently seen as a cortical based wedge-shaped bleed with the apex pointed medially
Posterior fossa bleeds (e.g. cerebellar ) may dissect into the brain stem (pons, cerebellar peduncles) or rupture into the fourth ventricle
Traumatic intracerebral hemorrhages may be seen immediately following an injury, most commonly occurring in areas where sudden deceleration of the head causes the brain to impact on bony prominences (temporal, frontal, occipital poles).
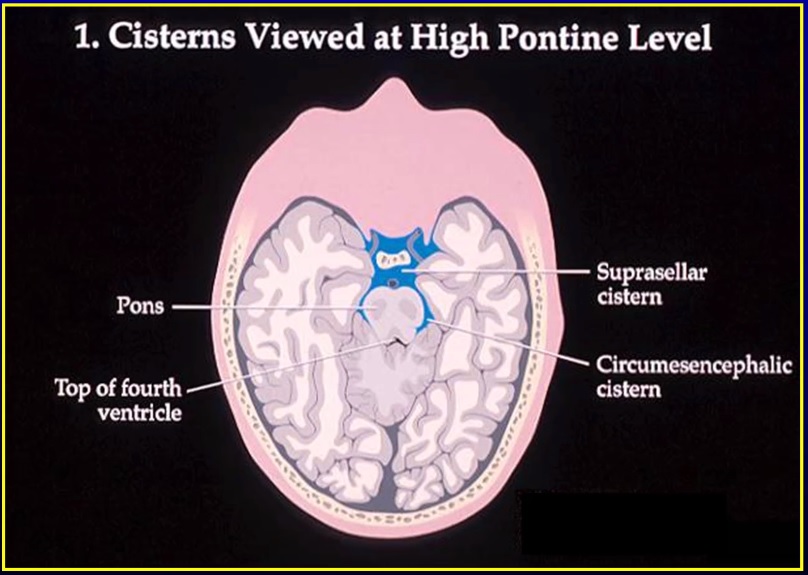
C(an) is for cisterns
There are two key questions to ask regarding the four key cisterns (Circummesencephalic, Suprasellar, Quadrigeminal and Sylvian)
Is there blood (subarachnoid hemorrhage)?
Are the cisterns open/is there high intracranial pressure?
Sagittal View Showing Key Levels of Cisterns
Evaluate if the circummesencephalic cistern is open or closed
Closure of the circummesencephalic cistern is one of the earliest signs of increased intracranial pressure (the
"canary in the coal mine")
80% of subarachnoid hemorrhages happen somewhere around the circle of willis/suprasellar cistern.
One of the earliest places to see hydrocephalus is on the temporal tips of the suprasellar cistern.
Scrutinize the sylvian cistern for two things:
Distal middle cerebral artery aneurysm (MCA)
A SAH here may only fill up this cistern with blood.
"Insular ribbon sign"
The insular ribbon is the end organ of the middle cerebral artery - it is the most distal brain perfused by the MCA.
Loss of gray white matter here is the earliest sign of MCA ischemia.
B(e) is for brain
Examine the brain for:
SYMMETRY
Make sure sulci and gyri appear the same on both sides.
Check for effacement of sulci (unilateral or bilateral).
GREY-WHITE DIFFERENTIATION
The earliest sign of a CVA on CT scan is the loss of the grey-white interface on CT scan (see next image below).
Compare one side to the contralateral side.
SHIFT
To evaluate for mass effect, evaluate a mid line structure (septum pellucidum) for shift.
The falx should be in the mid line with ventricles the same on both sides.
midline shift as measured from septum pellucidum (Arrow)
HYPER/HYPODENSITY
Blood, calcification and IV contrast are hyperdense (appear lighter) and air, fat and areas of tumor, ischemia are hypodense (appear darker).
CT BRAIN ON LEFT REVEALS MCA CLOT (Arrow); CT BRAIN ON RIGHT 2 DAYS LATER SHOWS HYPODENSE AREA OF INFARCT (arrow)
V(ery) is for ventricles/Vessels
CSF is produced in the lateral ventricles --> 3rd ventricle --> acqueduct of sylvius --> 4th ventricle at approximately 20 cc/hour. Look for:
Effacement
Shift
Blood
Examine the third, fourth and lateral ventricles for dilation or compression/shift.
dilated ventricles are seen on this CT brain. no GrEy-white differentiation or gyral PATTERN suggests this hydrocephalus IS ACUTE.
third ventricular hemOrrhage that has worked down into fourth ventricle, obstructING THE aquadeuct of sylvius and enlARGING THE temporal tips
Examine the vessels for signs of clot (hyperdense vessel)
HYPER DENSE sign/clot (circles) can OCCASIONALLY be seen in large vessel occlusion
B(ad) is for bone
Diagnosing skull fractures can be confusing due to the presence of sutures in the skull.
Skull fractures are divided into nondepressed (linear) or depressed fractures.
The presence of intracranial air on a CT scan means that the skull and dura have been violated at some point.
Non-aerated mastoid air cells suggest basilar skull fracture in petrous ridge.
The maxillary/ethmoid/sphenoid sinuses all should be visible and aerated: the presence of fluid in any of these sinuses in the setting of trauma should raise suspicion of a skull fracture.
Bone windowing on the right image gives greater resolution of depressed skull fracture
Non Aerated Mastoid air cells (circle) suggest basilar skull fracture in petrous bone
If no blood is seen, all cisterns are present and open, the brain is symmetric with normal grey- white differentiation, the ventricles are symmetric without dilation, the vessels are symmetric and not hyper-dense, and there is no fracture, there is no emeRgent diagnosis from the CT scan
tired of reading? Watch Dr. Perron teach how to read an emergent head ct
Referenes
1. Schreiger DL et al: Cranial computed tomography interpretation in acute stroke. JAMA
1998;279:1293-1297.
2. Perron AD et al: A multicenter study to improve emergency medicine residents’ recognition of intracranial emergencies on computed tomography. Ann Emerg Med 1998;32:554-562.
3. Leavitt MA et al: Abbreviated educational session improves cranial computed tomography scan interpretations by emergency physicians. Ann Emerg Med 1997;30:616-621.
4. Alfaro DA et al: Accuracy of interpretation of cranial computed tomography in an emergency medicine residency program. Ann Emerg Med 1995;25:169-174.
5. Roszler MH et al: Resident interpretation of emergency computed tomographic scans. Invest Radiol 1991;26:374-376. General Reference: Cwinn AA et al: Emergency CT scans of the head: a practical atlas. Mosby Year Book, St. Louis, 1998. Lee SH et al: Cranial MRI and CT, 4th ed. McGraw-Hill, New York, 1999.
Written and posted by Jeffrey A. Holmes, MD
Content and original authorship by Andrew Perron, MD, FACEP