When do we perform Transcutaneous pacing (TCP)?
Symptomatic clinically significant bradycardias
Don't just treat a number. Treat those bradycardias associated with hypotension, pulmonary edema, or evidence of decreased cerebral perfusion that is unresponsive to initial first line measure
Initiate TCP while searching for correctable causes and concomitantly administering other therapies (i.e. fluids, atropine, digibind, glucagon, high dose insulin)
Three common causes of bradycardia in the emergency department include drugs (specifically overdoses) hyperkalemia, and myocardial ischemia :
While most textbooks may quote overdrive pacing for refractory tachyarrhythmias, practically speaking, most of these will get simply get cardioverted
What about transvenous pacing (TVP)?
TCP is only a bridge until a transvenous pacemaker can be placed
There are a few instances where TCP may be preferable over TVP
Patients who have received thrombolytics
Patients who may respond to respond to therapy (eg. hyperkalemia, drug overdose)
Five Step Approach to Transcutaneous Pacing
Step 1: Apply the pacing electrodes and consider sedation (eg. versed)
Avoid placing the pads over an AICD or transdermal drug patches
There is little data on optimal placement however, try to place the pads as close as possible to the PMI (point of maximal impulse) [1,2]
Step 2: Turn on the monitor and set it to "pacing mode"
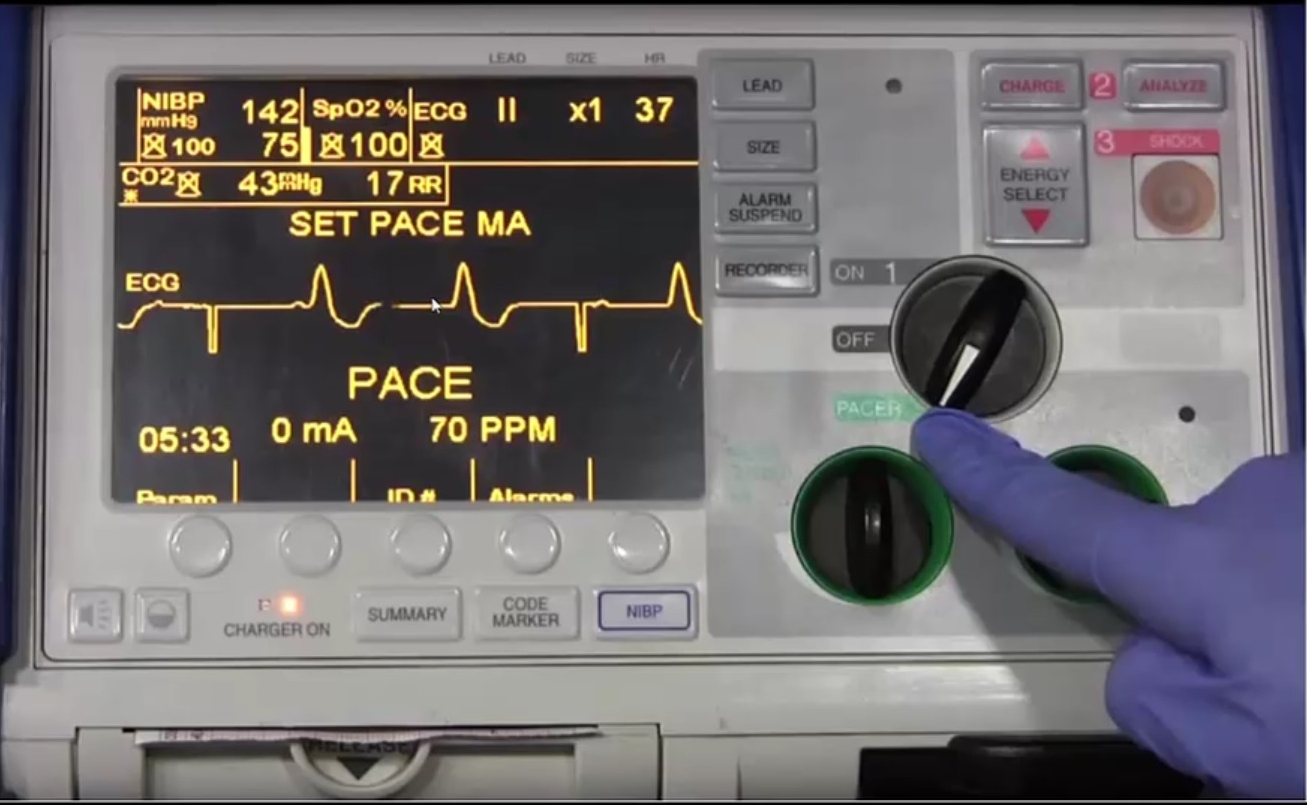
Step 3: Select the pacing rate using the rate button (generally 60-70 bpm is adequate)
Step 4: Increase current output from minimal until capture is achieved
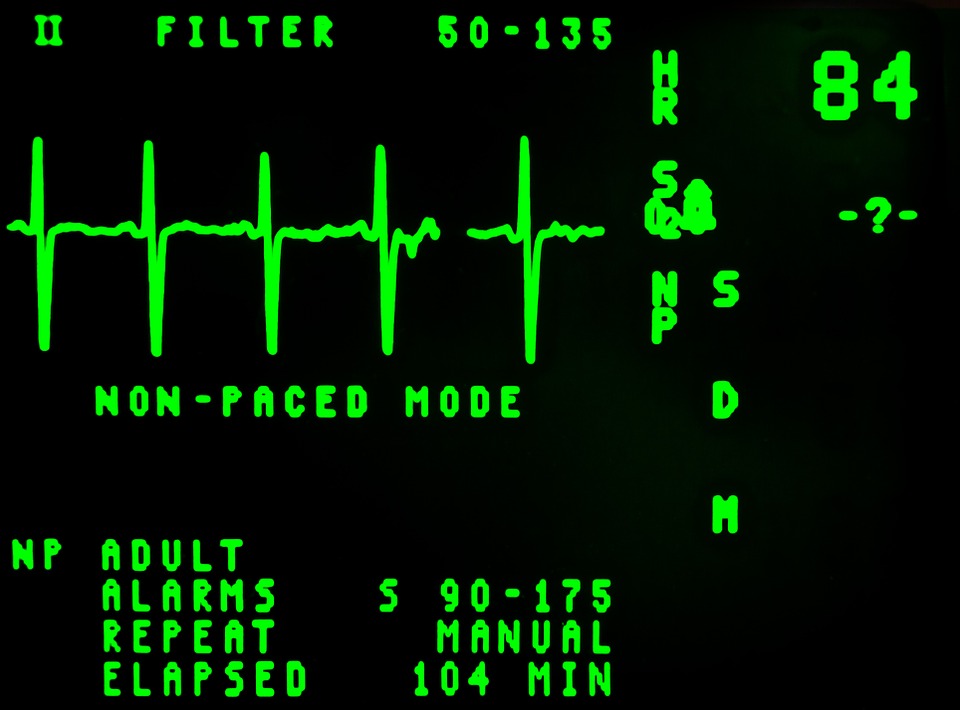
Below is an ECG with incomplete capture.
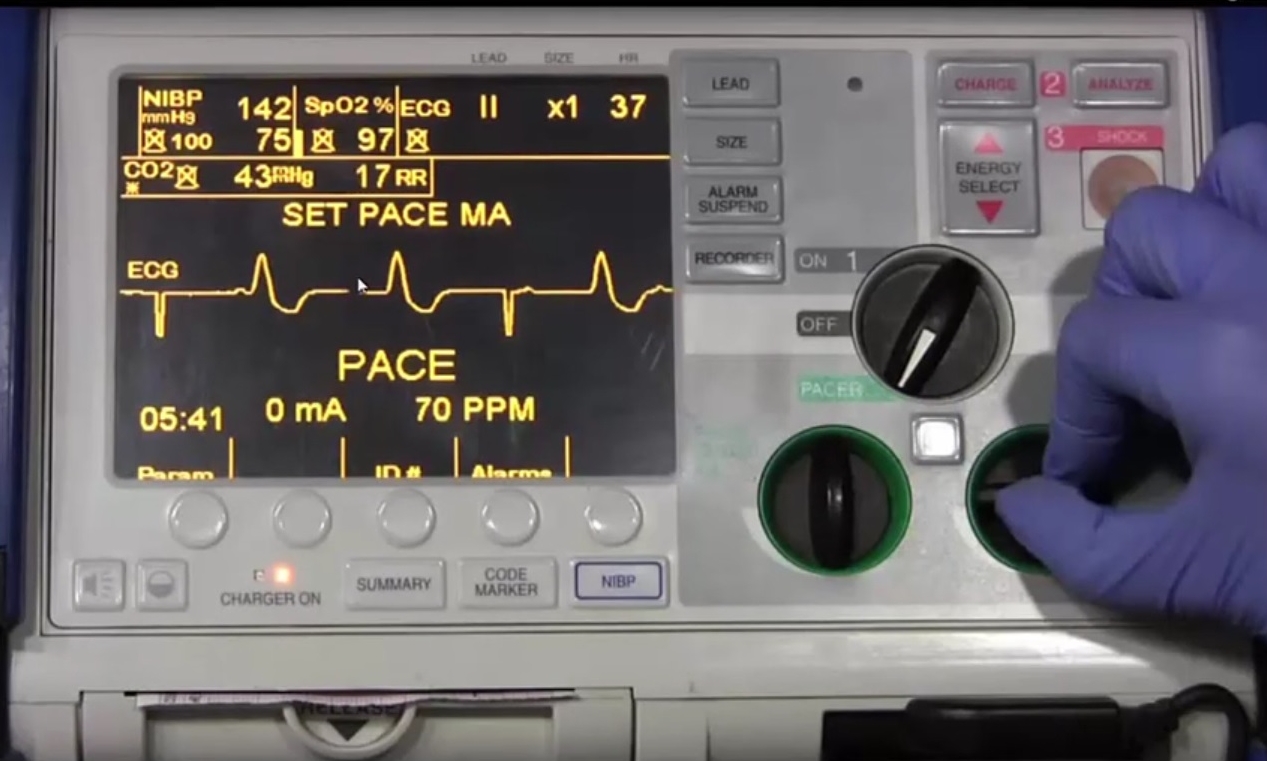
As the mA output is increased, complete capture is achieved.
Step 5: Confirm mechanical capture with pulse or ultrasound [3,4]
Complications
Induction of Vfib (rare)
Patient discomfort, burns (these are rare due to the large pads and lower outputs of today's TC pacing devices)
Failure to recognize an underlying treatable ventricular fibrillation due to obscuration of the ECG by pacer spikes
This can be troubleshooted by hitting the "cancellation button" on your monitor. This will pause the TCP spikes for a few seconds so you can identify the underlying rhythm.
Tired of Reading? Watch Jeff Holmes
discuss TC pacing in the ED
Written by Jeffrey A Holmes, MD
References
1. Panescu D, Webster J G, and Tompkins W J et al.: Optimisation of transcutaneous cardiac pacing by three-dimensional finite element modelling of the human thorax. Med Biol Eng Comput. 1995; 33: 769. [PMID: 8558949]
2. Webster J G, and Tompkins W J et al.: Optimisation of transcutaneous cardiac pacing by three-dimensional finite element modelling of the human thorax. Med Biol Eng Comput. 1995; 33: 769. [PMID: 8558949]
3. Ettin D and Cook T.: Using ultrasound to determine external pacer capture. J Emerg Med. 1999; 17:1007–1009. [PMID: 10595889]
4. Holger J S, Lamon R P, and Minnigan H J et al.: Use of ultrasound to determine ventricular capture in transcutaneous pacing. Am J Emerg Med. 2003; 21: 227. [PMID: 12811719]